Your cart is empty
What Type of Bariatric Surgery Has the Most Complications?

Bariatric surgery has become a popular solution for individuals struggling with obesity and related health conditions. It's a powerful tool that can lead to significant weight loss and improve many obesity-related conditions like type 2 diabetes, high blood pressure, heart disease, and more. However, like any surgical procedure, bariatric surgery comes with its risks and potential complications.
There are several types of bariatric surgery, including gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion with duodenal switch. Each procedure has its unique benefits and risks. It's important to note that the occurrence of complications can vary greatly depending on individual health factors, the skill and experience of the surgeon, and post-operative care and lifestyle changes.
Gastric Bypass
Roux-en-Y gastric bypass, commonly known as gastric bypass, is one of the most frequently performed weight loss surgeries worldwide. It's often referred to as the 'gold standard' of weight loss surgery due to its long history and extensive research supporting its effectiveness.

In this procedure, the surgeon creates a small pouch at the top of the stomach and connects this new pouch directly to the middle part of the small intestine (the jejunum), bypassing the rest of the stomach and the upper part of the small intestine (the duodenum). This dual mechanism of reducing stomach size and bypassing part of the small intestine results in less food intake and fewer calories absorbed, leading to significant weight loss.
Gastric bypass can lead to substantial improvements in obesity-related health conditions, such as type 2 diabetes, high blood pressure, sleep apnea, and more. However, it's also associated with several potential complications, including:
-
Dumping syndrome: This is a group of symptoms that occur when food, especially sugar, moves too quickly from the stomach pouch into the small intestine. Symptoms can include nausea, vomiting, bloating, diarrhea, dizziness, and rapid heart rate. Dumping syndrome can often be managed by adjusting the diet, such as avoiding high-sugar foods and eating smaller, more frequent meals.
-
Nutritional deficiencies: Because the procedure bypasses a part of the small intestine where many nutrients are absorbed, patients can develop deficiencies in nutrients such as iron, calcium, vitamin B12, and folate. To prevent these deficiencies, patients must adhere to a specific bariatric diet plan and take lifelong vitamin and mineral supplements.
-
Gastrointestinal leaks: A leak from the staple line in the stomach or the site where the small intestine is connected to the stomach pouch can occur. Though rare, this is a serious complication that can lead to infection and requires immediate medical attention. Treatment may involve antibiotics, drainage of the leaked fluid, or in severe cases, additional surgery.
-
Stricture or obstruction: This is a narrowing or blockage at the site where the small intestine is connected to the stomach pouch. Symptoms can include nausea, vomiting, and abdominal pain. Treatment usually involves a procedure to widen the narrowed area.
-
Gallstones: Rapid weight loss can lead to the formation of gallstones, which can cause abdominal pain and may require treatment.
Sleeve Gastrectomy
Sleeve gastrectomy, also known as vertical sleeve gastrectomy, is a surgical weight-loss procedure that involves removing approximately 80% of the stomach. The remaining portion of the stomach is a tubular pouch that resembles a banana, hence the name 'sleeve.'

This procedure significantly reduces the size of the stomach, limiting the amount of food that can be eaten at one time. It does not require rerouting or changing the order of the digestive system, which means it's a simpler operation compared to gastric bypass.
In addition to physically restricting the amount of food intake, sleeve gastrectomy also impacts gut hormones or the 'hunger hormones,' including ghrelin, which regulates hunger and satiety. The surgery leads to a significant reduction in the production of ghrelin, which can suppress hunger, reduce appetite, and enhance satiety.
Despite its benefits, sleeve gastrectomy is not without potential complications. These include:
-
Gastroesophageal reflux disease (GERD): GERD is a chronic condition where stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). Some patients may experience an increase in GERD symptoms after sleeve gastrectomy. This can cause symptoms such as heartburn, acid reflux, and in some cases, it can lead to more serious complications like esophagitis or Barrett's esophagus.
-
Stomach leaking: One of the more serious complications of sleeve gastrectomy is a gastric leak, which occurs when the staple line used to create the new stomach pouch leaks fluid. This can happen if the staples don't hold, or if the tissue is weak or becomes damaged. Gastric leaks can lead to infection and are typically treated with antibiotics, although in severe cases, additional surgery may be required.
-
Sleeve stricture or stenosis: This is a rare complication where the new stomach sleeve becomes too narrow, making it difficult for food and liquid to pass to the rest of the digestive tract. Symptoms include nausea, vomiting, and difficulty swallowing. Treatment usually involves a procedure to widen the narrowed area.
-
Nutritional deficiencies: While less common than in gastric bypass, deficiencies can still occur due to reduced food intake and alterations in gut hormones. Patients are typically advised to take vitamin and mineral supplements to prevent deficiencies.
Adjustable Gastric Band
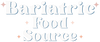
The adjustable gastric band, often known by the brand name Lap-Band, is a type of weight loss surgery that involves placing a silicone band around the upper part of the stomach. This creates a small pouch above the band, with the rest of the stomach below. The band is connected to a port under the skin of the abdomen, and can be tightened or loosened by injecting or removing saline solution, thereby controlling the size of the opening from the pouch to the rest of the stomach.

This procedure works primarily by restricting the amount of food that can be consumed at one time. Because the upper pouch can hold only a small amount of food, you feel full more quickly and therefore eat less.
One of the advantages of the adjustable gastric band is that it's less invasive than other forms of bariatric surgery. There's no cutting or stapling of the stomach, and no rerouting of the intestines. The procedure is also reversible - if necessary, the band can be removed, returning the stomach to its original form.
However, the adjustable gastric band is not without potential complications. These include:
-
Band slippage or erosion: Over time, the band can slip out of place, causing the upper pouch to become larger than intended. This can lead to problems such as heartburn, vomiting, and difficulty swallowing. In some cases, the band can erode into the stomach, which can cause pain and may require additional surgery to remove or reposition the band.
-
Esophageal dilation: This can occur if you overeat or eat too quickly, causing the esophagus to stretch. Over time, this can lead to difficulty swallowing and other complications.
-
Inadequate weight loss or weight regain: Some patients may not lose weight as effectively with the gastric band compared to other procedures. There's also a risk of weight regain if the band is not properly adjusted, or if the patient does not adhere to the recommended dietary guidelines.
-
Band malfunction: The band or the port can malfunction, leading to a leak in the system or difficulty adjusting the band. This may require additional surgery to fix.
-
Gastroesophageal reflux disease (GERD): Some patients may experience an increase in GERD symptoms after the procedure.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is a complex bariatric surgery that combines two surgical techniques: restrictive and malabsorptive. The restrictive part involves removing about 70% of the stomach along the greater curvature to create a tubular gastric sleeve, which restricts food intake. The malabsorptive part involves rerouting a significant portion of the small intestine to create two separate pathways and one common channel.
The shorter digestive pathway carries food from the stomach to the common channel, and the longer pathway carries bile and pancreatic enzymes from the liver and pancreas to the common channel. The food and digestive juices interact only in the common channel, significantly reducing the opportunity to absorb calories and nutrients, leading to substantial weight loss.
BPD/DS leads to significant improvements in obesity-related conditions, including type 2 diabetes, high blood pressure, high cholesterol, and sleep apnea. However, it also carries the highest risk of complications among all bariatric surgeries. These include:
-
Malnutrition and vitamin deficiencies: Because a large part of the small intestine is bypassed, patients can develop severe nutritional deficiencies. These can affect a wide range of nutrients, including protein, fat, vitamins, and minerals, and can lead to conditions such as anemia and osteoporosis. To prevent these deficiencies, patients must take lifelong bariatric vitamin and mineral supplements and have regular check-ups to monitor their nutritional status.
-
Chronic diarrhea and foul-smelling stools: The changes to the digestive system can lead to these unpleasant side effects. The rapid transit of food through the digestive tract can cause loose, greasy, foul-smelling stools, a condition known as steatorrhea. This can be difficult to manage and may impact the patient's quality of life.
-
Higher mortality rate: Due to the complexity of the procedure and the risk of serious complications, BPD/DS has a higher mortality rate compared to other bariatric surgeries. However, it's important to note that the overall risk is still low, and the procedure is typically reserved for individuals with severe obesity or those who haven't achieved adequate weight loss from other bariatric surgeries.
-
Stomach and intestinal ulcers: These can develop in the stomach pouch or the small intestine, especially in patients who smoke or take nonsteroidal anti-inflammatory drugs (NSAIDs).
-
Protein-calorie malnutrition: This is a rare but serious complication that can occur if the common channel is too short, leading to severe protein deficiency.
Conclusion
Choosing to undergo bariatric surgery is a significant decision that can dramatically affect your health and lifestyle. Each type of surgery has its own set of benefits and risks, and it's crucial to consider these carefully. While some procedures may lead to more significant weight loss, they may also carry a higher risk of complications.
The adjustable gastric band and sleeve gastrectomy are less invasive options with lower complication rates, but they may not result in as much weight loss or improvement in obesity-related conditions as the more complex gastric bypass or BPD/DS.
In the end, the choice of which type of bariatric surgery to undergo should be made in close consultation with your doctor, considering your individual health status, weight loss goals, and willingness to adhere to the necessary lifestyle changes.
Author: Joey Young Joey is a writer and researcher with a big passion for health. As a dad to five kids and three dogs, he knows first-hand the importance of a healthy lifestyle. His work is all about sharing useful health advice and insights with readers from all walks of life. |
Reviewed By: Dr. K. Huffman Dr. Kevin D. Huffman, D.O., is a board-certified bariatric physician with a distinguished reputation in obesity treatment. As the founder of American Bariatric Consultants, he has impacted over 10,000 patients and trained numerous healthcare providers. His protocols and training materials have made him a national leader in bariatric medicine. |
Bariatric Guides & Information
More Info
Customer Favorites
- Choosing a selection results in a full page refresh.